Report Materials
WHY WE DID THIS STUDY
This study continues OIG's body of work examining overpayments made by Medicare. Overpayments can be identified by a number of key players including providers and Medicare contractors. Recovering overpayments is critical to reducing improper payments in the Medicare program. Past OIG work found that overpayments referred by program safeguard contractors (PSCs) for collection did not result in significant recoveries to the Medicare program. As of 2012, CMS had transitioned the workload of most PSCs to six zone program integrity contractors (ZPICs). In 2016, CMS began transitioning the remaining PSCs and ZPICs to unified program integrity contractors (UPICs). OIG's work on both PSCs and ZPICs identified deficiencies in how contractors were tracking and reporting overpayment data. This study provides an update on the collection of ZPIC- and PSC-referred overpayments and identifies ongoing challenges that contractors face in tracking and collecting overpayments identified by ZPICs and PSCs.
HOW WE DID THIS STUDY
Our study focused on overpayments that ZPICs and PSCs sent to Medicare administrative contractors (MACs) for collection in fiscal year (FY) 2014. We collected and analyzed overpayment referral and collection data from ZPICs, PSCs, and MACs. We also surveyed ZPICs, PSCs, and MACs to understand their procedures for tracking overpayment referrals and collections as well as barriers and challenges they face in performing these tasks.
WHAT WE FOUND
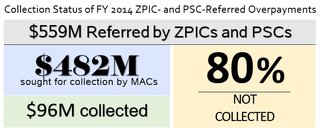
ZPICs and PSCs are key players in identifying Medicare overpayments, and they referred $559 million in overpayments in FY 2014 to the MACs responsible for collecting overpayments. The dollars referred varied widely across ZPICs and PSCs, with just 2 of 10 contractors identifying half of the total overpayment dollars. Based on ZPIC and PSC referrals, MACs sought to collect $482 million but collected only $96 million, or 20 percent; 80 percent remained uncollected as of September 30, 2015. Although the collection rate remains low, it is almost three times the 7-percent collection rate for PSC identified overpayments that OIG found in its 2010 review when only PSCs were in existence. MACs' collection rates ranged from a low of 11 percent for home health and hospice overpayments to a high of 59 percent for Part A overpayments referred by ZPICs and PSCs. We found that ZPICs, PSCs, and MACs continue to experience challenges in tracking referrals and collections of overpayments. In particular, the number and amount of overpayment referrals reported by ZPICs and PSCs often did not match to what was reported by MACs-with discrepancies totaling $130 million. Furthermore, ZPICs, PSCs, and MACs used different report formats, which can lead to difficulty in tracking overpayment referrals.
WHAT WE RECOMMEND
We recommend that CMS identify and implement strategies to increase the identification of overpayments as well as MACs' collection of ZPIC and UPIC referred overpayments. To increase collections, CMS should implement the surety bond requirement for home health providers and consider surety bonds for other providers based on their level of risk. Furthermore, we recommend that CMS improve the ability of ZPICs, UPICs, and MACs to track overpayment referrals and collections by creating a standard report format for all contractors and requiring ZPICs, UPICs, and MACs to use a unique identifier for each overpayment. CMS concurred with all of our recommendations except the one regarding surety bonds. CMS did not concur or non-concur with this recommendation; it stated that it is evaluating how to effectively implement the surety bond requirement while avoiding undue provider burden.
View in Recommendation Tracker
Notice
This report may be subject to section 5274 of the National Defense Authorization Act Fiscal Year 2023, 117 Pub. L. 263.