Report Materials
Correction Notice
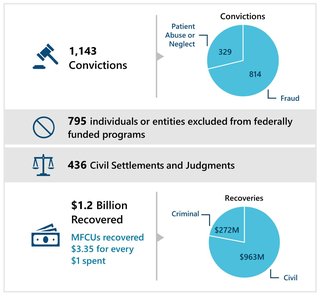
This report was originally posted on March 14, 2024. OIG discovered that the report contained numerical errors. We have corrected the errors and posted the corrected report on May 17, 2024; please use this version. The earlier report stated OIG imposed a total of 2,112 exclusions on individuals and entities and that MFCU cases were responsible for 850 (40 percent) of those exclusions. The correct numbers are that OIG imposed a total of 2,112 exclusions on individuals and entities and MFCU cases were responsible for 795 (38 percent) of those exclusions.
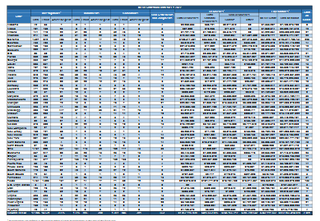
Medicaid Fraud Control Units (MFCUs) investigate and prosecute Medicaid provider fraud and patient abuse or neglect. The Department of Health and Human Services Office of Inspector General (OIG) is the designated Federal agency that oversees and annually recertifies and approves Federal funding for each MFCU. For this report, OIG analyzed the annual statistical data on case outcomes (such as convictions; civil settlements and judgments; and recoveries) that 53 MFCUs submitted to OIG for fiscal year 2023, as well as other historical data. Those MFCUs operated in all 50 States, the District of Columbia, Puerto Rico, and the U.S. Virgin Islands.
Notice
This report may be subject to section 5274 of the National Defense Authorization Act Fiscal Year 2023, 117 Pub. L. 263.