Report Materials
Why OIG Did This Audit
- In March 2020, Congress enacted the Families First Coronavirus Response Act in response to the COVID-19 public health emergency, which required States to ensure that most individuals were continuously enrolled for Medicaid benefits (enrollees).
- The Consolidated Appropriations Act, 2023, ended the continuous enrollment condition. As a result, States had to conduct renewals, post-enrollment verifications, and redeterminations (Medicaid eligibility actions) for all enrollees, including terminating Medicaid enrollment of ineligible individuals.
- This audit of California is part of a series of audits examining whether States completed Medicaid eligibility actions during the unwinding period in accordance with Federal and State requirements.
What OIG Found
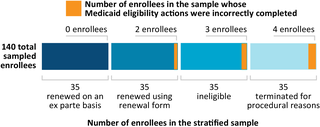
Of the 1,830,923 enrollees who had their Medicaid eligibility renewed or coverage terminated during April 1 through August 31, 2023 (audit period), we sampled 140 enrollees and determined that California incorrectly completed Medicaid eligibility actions for 9 enrollees.
On the basis of our sample results, we estimated that California incorrectly renewed eligibility or incorrectly terminated coverage for 78,853 of the 1,830,923 enrollees during our audit period.
What OIG Recommends
We recommend that California: (1) redetermine eligibility for the sampled enrollees that we identified as having incorrect eligibility determinations, (2) provide caseworkers additional training to reduce errors, (3) revise its guidance to instruct counties to document in case files essential information to support enrollees’ continuing eligibility, and (4) identify and correct the system issues that caused incorrect Medicaid eligibility actions. The full recommendations are in the report.
California concurred with all our recommendations and described actions that it planned to take to address them.
View in Recommendation Tracker
Notice
This report may be subject to section 5274 of the National Defense Authorization Act Fiscal Year 2023, 117 Pub. L. 263.