Report Materials
Key Takeaways
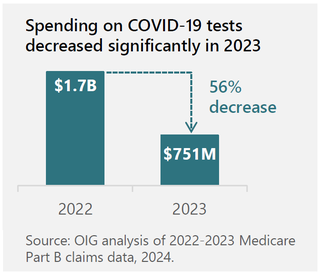
- In 2023, total Medicare Part B spending on clinical diagnostic laboratory tests (lab tests) decreased by 5.4 percent from total lab test spending in 2022.
- Spending on COVID-19 tests decreased significantly in 2023 due to several factors, including the widespread availability of over-the-counter COVID-19 tests.
- Medicare Part B spending on genetic tests has steadily increased over the last 10 years.
Why OIG Did This Review
This review is part of an effort to help control Medicare lab test spending. The Protecting Access to Medicare Act of 2014 required that Medicare Part B payment rates align with rates paid by private payors. To provide oversight that these efforts were helping to control lab test spending, Congress also mandated that OIG publicly release an annual analysis of the top 25 tests based on Medicare spending and conduct analyses that OIG determines appropriate. This data snapshot provides an analysis of Medicare Part B payments for lab tests in 2023, including an analysis of the top 25 tests. From 2018 through 2020, CMS implemented new Medicare Part B lab test payment rates. In 2021, new payment rates were to go into effect; however, changes in legislation have delayed any rate changes. The next payment rate changes are scheduled for January 1, 2027.
What OIG Did
We analyzed Medicare Part B claims data for lab tests paid for under the Medicare Clinical Laboratory Fee Schedule in 2023. We identified key statistics and trends for total Medicare Part B spending on lab tests, including the top 25 lab tests on the basis of total spending.
What OIG Recommends
This data snapshot contains no recommendations.
Notice
This report may be subject to section 5274 of the National Defense Authorization Act Fiscal Year 2023, 117 Pub. L. 263.